| Oregon Medical Power of Attorney Form |
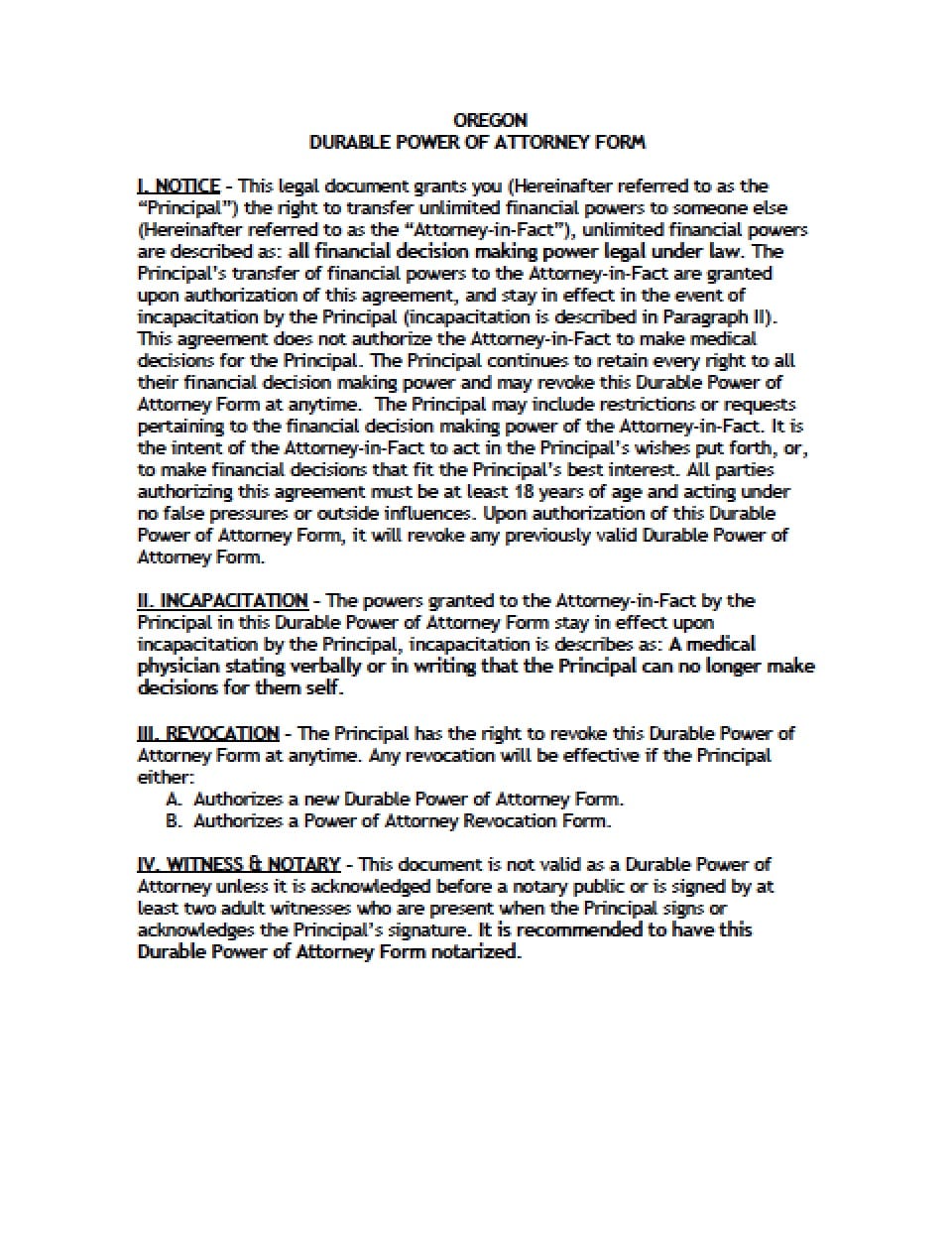
The Oregon Medical Power of Attorney Form is a document that is designed to provide a Principal, the necessary documentation so that they may transfer powers of their health care to someone else, better known as an Agent or an Attorney In Fact. This document, inasmuch as it is a legal document that is meant to protect the Principal, if it’s not well composed, could significantly affect the Principal’s financial and real property and how it could be affected at the time that distribution begins. Therefore it’s very important that the Principal trusts the Agent that they select and be certain to discuss the Principal’s options with the Agent prior to completing the document.
This document requires that all signatories be present to sign the document in the witness of a licensed Notary or two witnesses. The Principal has the right to revoke this document at their discretion, providing notice is provided in writing and is delivered or served to the Agent(s).
How to Write
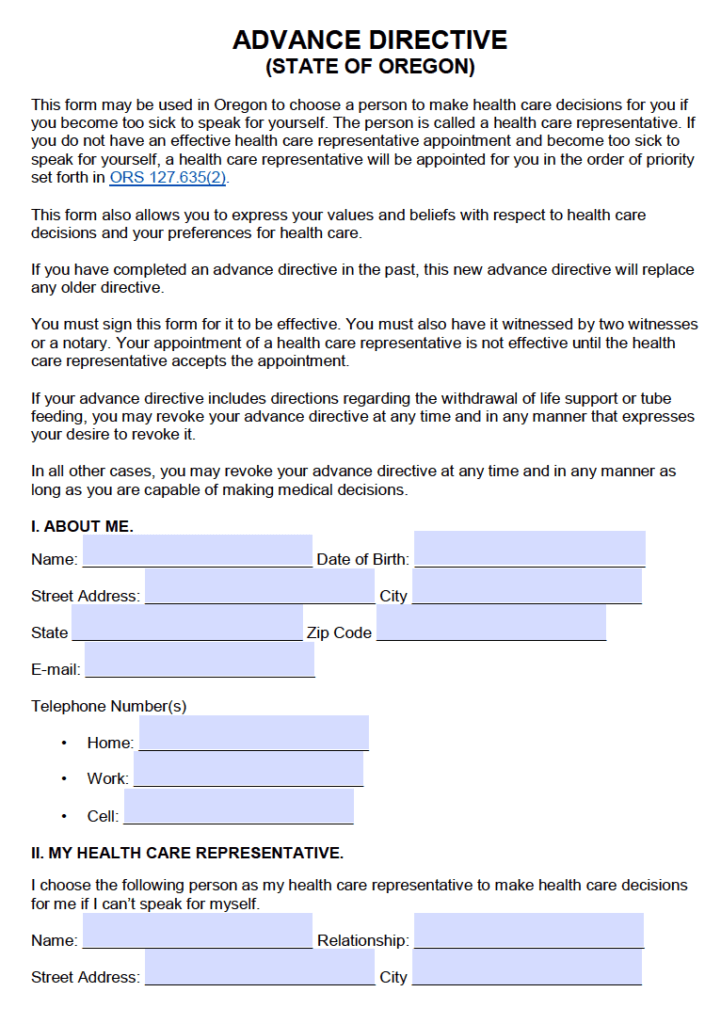
1 – Download The Template To Issue An Advanced Health Care Directive In Oregon Here
You can find the paperwork to develop and execute a Health Care Directive in this state can be saved to your machine directly from this page. Two optional file versions are available to decide from: Adobe PDF and MS Word. You may access either or both file types by clicking the appropriately labeled button just beneath the title of this page. Some information may be filled out on screen with a compatible editing program but ultimately, the acting Principal (the Patient) will need to actively make his or her wishes known by directly initialing certain options.
2 – The Patient Must Be Clearly Identified
The Patient issuing this document will be considered the Principal in the Principal-Agent relationship. He or she must have a clear understanding of the type of authority being delivered here. Due to the sensitive nature of this paperwork, the same individual we name in “I. About Me,” must be the same signature party issuing this paperwork. We will begin identifying the Patient by reporting his or her full legal name on the blank line labeled “Name” in the first article of this paperwork. Note: The name you enter here must be presented exactly as it appears on the Patient’s I.D. cards (i.e. insurance cards, driver’s license) and his or her paperwork with medical care institutions. 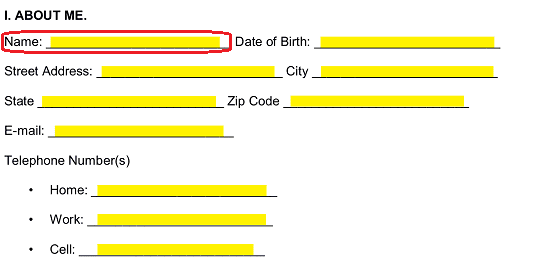 Oftentimes, a medical facility will need more than just a Patient’s name to verify his or her identity. Thus, we must provide some additional information to define this Principal entity. Use the blank line labeled “Date Of Birth” to fill in the month, two-digit calendar day, and four-digit calendar year of the Patient’s birth date.
Oftentimes, a medical facility will need more than just a Patient’s name to verify his or her identity. Thus, we must provide some additional information to define this Principal entity. Use the blank line labeled “Date Of Birth” to fill in the month, two-digit calendar day, and four-digit calendar year of the Patient’s birth date. 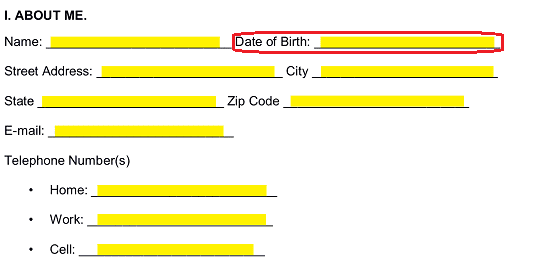 The next four blank spaces will serve to report the Patient’s address as it appears in his or her I.D. Use the “Street Address” space to record the building number, street or road name/number, and any applicable apartment number listed on the Patient’s I.D. as part of his or her address.
The next four blank spaces will serve to report the Patient’s address as it appears in his or her I.D. Use the “Street Address” space to record the building number, street or road name/number, and any applicable apartment number listed on the Patient’s I.D. as part of his or her address. 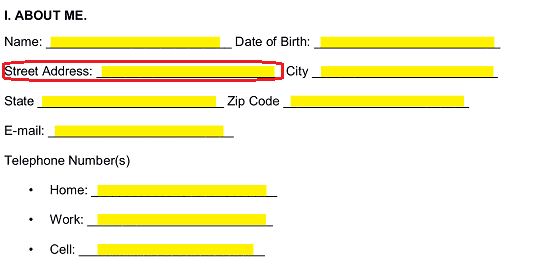 The “City,” “State,” and “Zip Code” lines have been reserved for the remainder of the Patient’s address to be reported. Make sure this information is accurate.
The “City,” “State,” and “Zip Code” lines have been reserved for the remainder of the Patient’s address to be reported. Make sure this information is accurate. 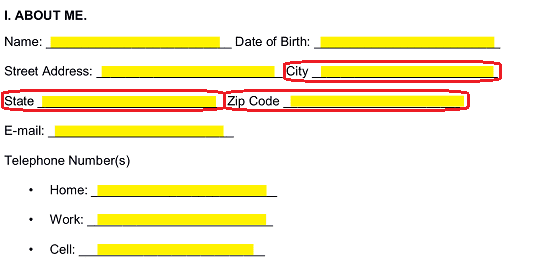 The remainder of this section will call for the Patient’s “E-Mail” address and “Telephone Number(s)” to be documented. Note that a separate space has been included for the Patient’s “Home” phone number, “Work” phone number, and “Cell” phone number. It is recommended that you double check your references as this information must be up-to-date and accurate.
The remainder of this section will call for the Patient’s “E-Mail” address and “Telephone Number(s)” to be documented. Note that a separate space has been included for the Patient’s “Home” phone number, “Work” phone number, and “Cell” phone number. It is recommended that you double check your references as this information must be up-to-date and accurate. 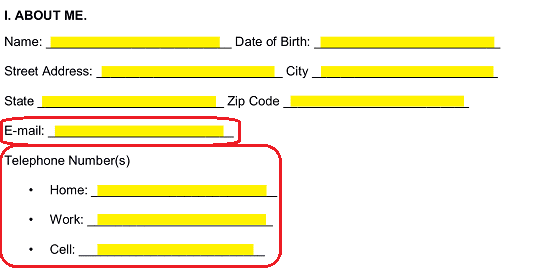
3 – Formally Name Each Health Care Representative Intended To Hold Principal Authority
The Health Care Representative who physicians will be expected to turn to when the Patient has been incapacitated or rendered unable to act or communicate in an effective manner must be presented in “II. My Health Care Representative.” The first blank space here (labeled “Name”) has been reserved for the full name of this person. It is imperative to the function of this paperwork that this name is recorded exactly as it appears on the Agent’s I.D. cards (i.e. Passport, Driver’s License). 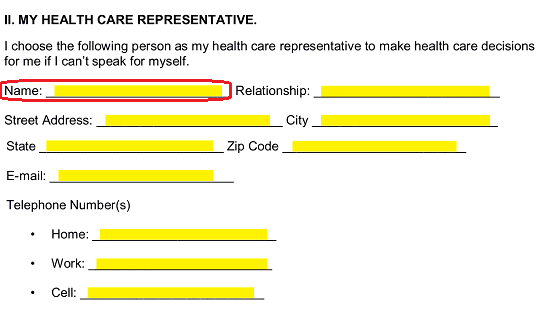 Naturally, any entity in charge of the Patient’s health care will want to know the “Relationship” the elected Health Care Representative holds with the Patient when this document is employed. This question is nicely handled by simply reporting the nature of the Health Care Agent’s relationship to the Principal/Patient on the second blank space in this section.
Naturally, any entity in charge of the Patient’s health care will want to know the “Relationship” the elected Health Care Representative holds with the Patient when this document is employed. This question is nicely handled by simply reporting the nature of the Health Care Agent’s relationship to the Principal/Patient on the second blank space in this section. 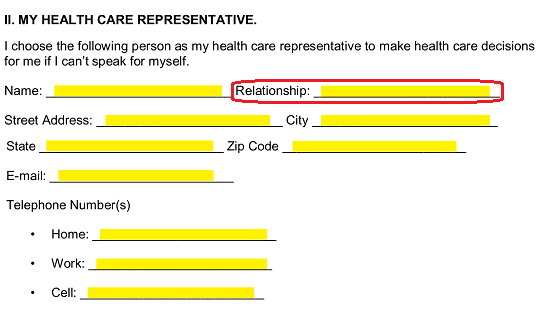 The complete address of the Health Care Representative must also be documented in the second section. Use the spaces bearing the labels “Street Address,” “City,” “State,” and “Zip Code” to produce this information. Naturally we will need to make sure this information is identical to the Agent’s I.D. cards.
The complete address of the Health Care Representative must also be documented in the second section. Use the spaces bearing the labels “Street Address,” “City,” “State,” and “Zip Code” to produce this information. Naturally we will need to make sure this information is identical to the Agent’s I.D. cards. 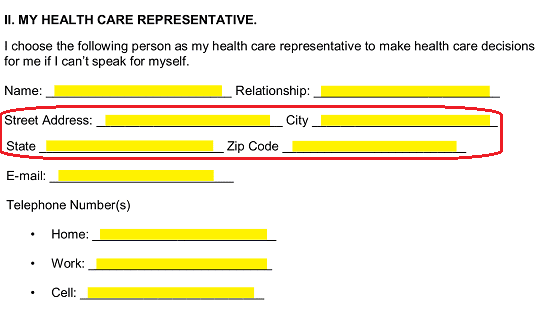
Report the “E-Mail” address of the Health Care Representative on the next blank line. In many cases, this may be how medical information regarding the Patient is dispensed so make sure this is a secure and well-maintained address. 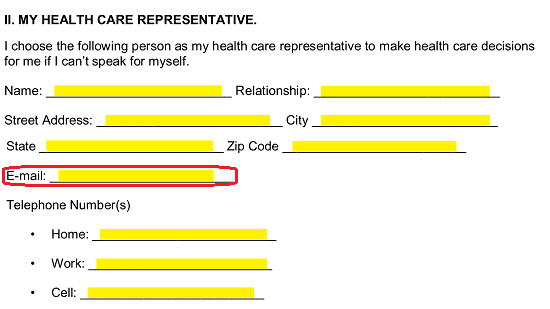
Usually, the first point of contact between a health care institution and the Health Care Representative, when the Patient suffers a traumatic medical event, will be through a telephone call. When this happens, it can be considered crucial that the Health Care Representative is reachable on a fairly immediate basis. Enter his or her “Home” telephone number, his or her telephone number at “Work” (include any relevant extensions or instructions), and his or her “Cell” phone number on the three blank lines under the heading “Telephone Number(s)” in this section. 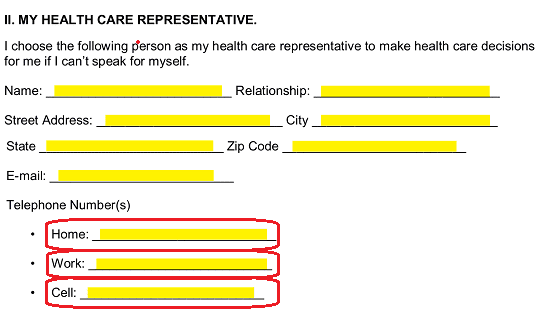 Sometimes, a Health Care Representative is simply not reachable, available, or willing to live up to the expectations of the Patient in relation to these directives. Thus, a wise precaution against such a possibility is to have an Alternate Health Care Representative set in place to make sure the Patient’s preferences and expectations are understood and safeguarded. Locate item “A.) First Alternate Health Care Representative” then, fill in the full name of the Alternate Health Care Representative who should be contacted as a replacement for the Health Care Representative you named above.
Sometimes, a Health Care Representative is simply not reachable, available, or willing to live up to the expectations of the Patient in relation to these directives. Thus, a wise precaution against such a possibility is to have an Alternate Health Care Representative set in place to make sure the Patient’s preferences and expectations are understood and safeguarded. Locate item “A.) First Alternate Health Care Representative” then, fill in the full name of the Alternate Health Care Representative who should be contacted as a replacement for the Health Care Representative you named above. 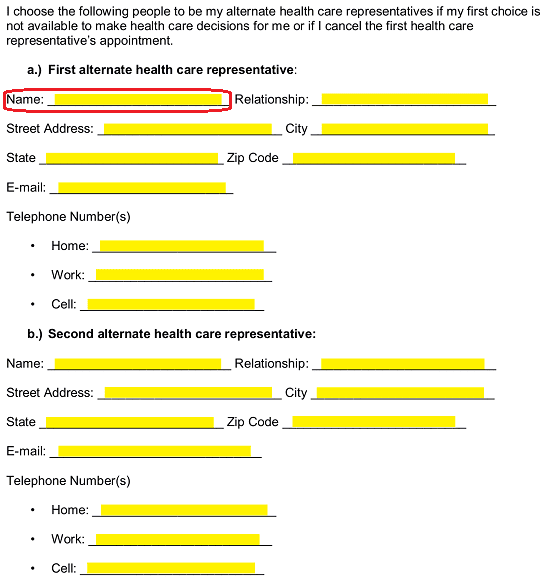 Disclose the “Relationship” the First Alternate Health Care Representative holds with the Patient on the blank space adjacent to his or her name.
Disclose the “Relationship” the First Alternate Health Care Representative holds with the Patient on the blank space adjacent to his or her name. 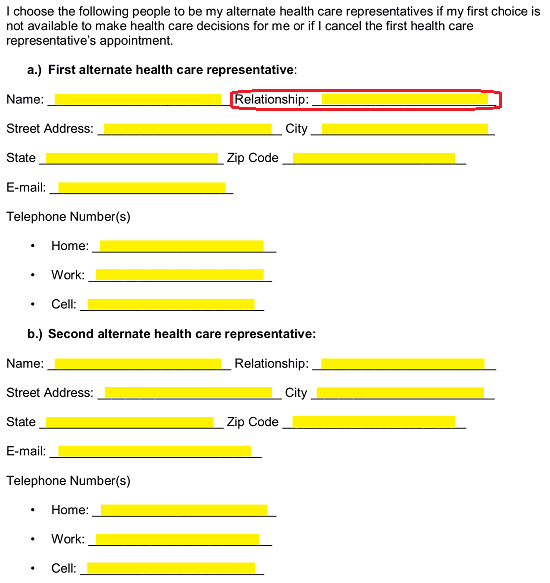 Utilize the next four blank spaces to document the First Alternate Health Care Representative’s complete address.
Utilize the next four blank spaces to document the First Alternate Health Care Representative’s complete address. 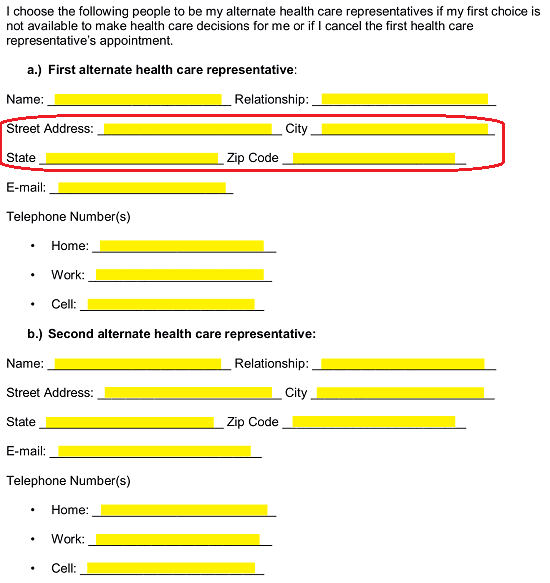 Finally, supply the First Alternate Health Care Representative’s “E-Mail” address and “Telephone Number(s)” using the space provided in item “A.) First Alternate Health Care Representative.”
Finally, supply the First Alternate Health Care Representative’s “E-Mail” address and “Telephone Number(s)” using the space provided in item “A.) First Alternate Health Care Representative.” 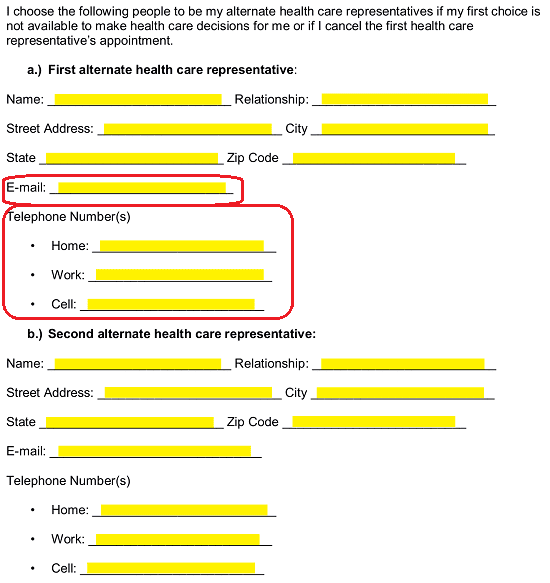 An additional item, “B.) Second Alternate Health Care Representative,” has been included so that a second person can be named with the power to make the medical decisions and take the actions the Patient would want taken on his or her behalf should both the Health Care Representative and First Alternate Health Care Representative are both unavailable or unable to fulfill their rolls. This section will provide distinct areas where you can record the Second Alternate Health Care Representative’s “Name,” “Relationship” to the Patient, “Street Address,” “City,” “State,” “Zip Code,” “E-Mail” address,” and “Telephone Number(s).” If the Patient has not named such an entity, you may leave it blank though it should be kept in mind that many would consider it wise to have such an entity documented and formally named with power.
An additional item, “B.) Second Alternate Health Care Representative,” has been included so that a second person can be named with the power to make the medical decisions and take the actions the Patient would want taken on his or her behalf should both the Health Care Representative and First Alternate Health Care Representative are both unavailable or unable to fulfill their rolls. This section will provide distinct areas where you can record the Second Alternate Health Care Representative’s “Name,” “Relationship” to the Patient, “Street Address,” “City,” “State,” “Zip Code,” “E-Mail” address,” and “Telephone Number(s).” If the Patient has not named such an entity, you may leave it blank though it should be kept in mind that many would consider it wise to have such an entity documented and formally named with power. 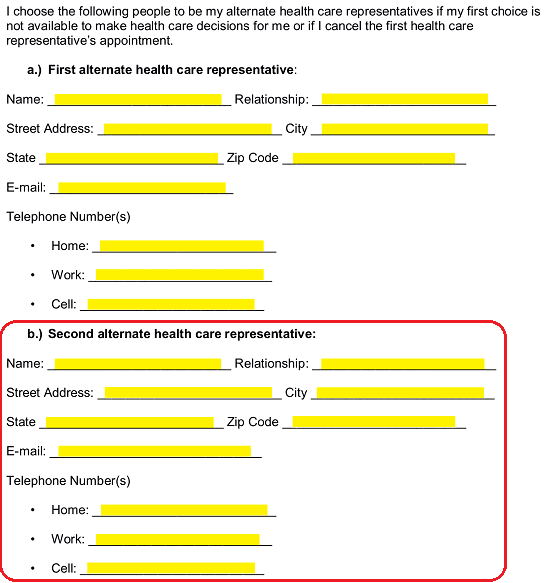
4 – Define The Level Of Authority Being Delivered Here
The Patient who intends to grant the right to represent him or her to a Health Care Representative will need to review section “III. Instructions To My Health Care Representative.” This area will give the Patient the opportunity to quickly and decisively report how much authority the Health Care Representative will be able to wield in the Patient’s name. The Patient must initial one of the statements in this section before proceeding.
If the Patient expects the Health Care Representative to follow his or her directives exactly as they have been delivered (and literally) then the Patient must initial the blank line labeled “To The Extent Appropriate.” 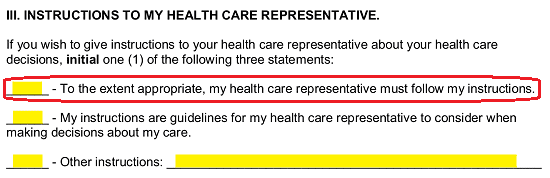 If the Patient wishes the Health Care Representative to use his or her instructions as “Guidelines” when called upon to make a medical decision on his or her behalf, then the Patient must initial the blank space attached to the words “My Instructions Are Guidelines…”
If the Patient wishes the Health Care Representative to use his or her instructions as “Guidelines” when called upon to make a medical decision on his or her behalf, then the Patient must initial the blank space attached to the words “My Instructions Are Guidelines…” 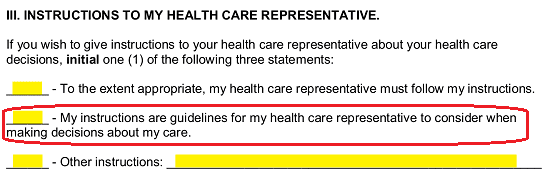 If the Patient would like to deliver a more descriptive narrative of the level of authority the Health Care Representative should hold then he or she should initial the blank line labeled “Other Instructions.” Once this is done the instructions, he or she have may be entered directly on the blank line provided or it may be supplied through an attachment that is dated and signed by the Patient.
If the Patient would like to deliver a more descriptive narrative of the level of authority the Health Care Representative should hold then he or she should initial the blank line labeled “Other Instructions.” Once this is done the instructions, he or she have may be entered directly on the blank line provided or it may be supplied through an attachment that is dated and signed by the Patient. 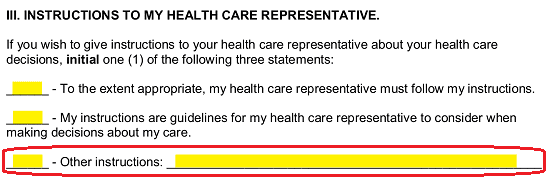
5 – A Record Of The Patient’s End-Of-Life Care Preferences Should Be Provided
The next section, titled “IV. Directions Regarding My End Of Life Care,” will begin by presenting some very valuable information and definitions. The Patient should read this area to his or her comprehension then continue to the item labeled “A. Statement Regarding End Of Life Care.” If the Patient does not wish to receive life support procedures necessary to prevent death, then he or she must initial the blank line just before the paragraph beginning with “I Do Not Want My Life To Be Prolonged…” If the Principal wishes to explain this further by naming specific scenarios where life support should be prevented, then you may either use the available space to list them or provide such a report in an attachment. 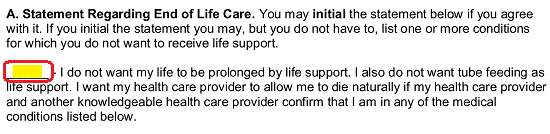 The next section, “B. Additional Directions Regarding End Of Life Care” will also present some choices aimed at documenting the Principal’s preferences when he or she is an incapacitated Patient near the end of his or her life. In “I.) Close To Death,” the Patient will need to initial the first, second, or third statement to indicate his or her feelings regarding being tube fed (given food in a liquid suspension through a tube) when all such a treatment will result in is prolonging the moment of death. He or she should initial the first statement “…To Receive Tube Feeding,” the second statement if tube feeding should only occur as the physician recommends, or the third statement if he or she does not wish to be tube fed.
The next section, “B. Additional Directions Regarding End Of Life Care” will also present some choices aimed at documenting the Principal’s preferences when he or she is an incapacitated Patient near the end of his or her life. In “I.) Close To Death,” the Patient will need to initial the first, second, or third statement to indicate his or her feelings regarding being tube fed (given food in a liquid suspension through a tube) when all such a treatment will result in is prolonging the moment of death. He or she should initial the first statement “…To Receive Tube Feeding,” the second statement if tube feeding should only occur as the physician recommends, or the third statement if he or she does not wish to be tube fed. 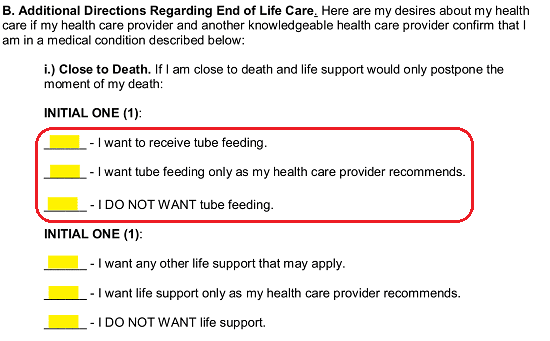 Another issue that should be dealt with at the end of one’s life is life support. The next three statements provide a choice regarding how the option of life support should be treated. If the Patient wishes his or her life prolonged even if that means he or she will be purely dependent upon machinery to live, then the Patient should initial the statement “I Want Any Other Life Support…” If he or she only wishes life support to be administered at the discretion of the Health Care Provider in charge of his or her care, then the Patient must initial the statement “I Want Life Support…” If the Patient is at the end of his or her life and wants to be allowed to die naturally, then he or she should initial the blank line attached to the words “I Do Not Want Life Support.”
Another issue that should be dealt with at the end of one’s life is life support. The next three statements provide a choice regarding how the option of life support should be treated. If the Patient wishes his or her life prolonged even if that means he or she will be purely dependent upon machinery to live, then the Patient should initial the statement “I Want Any Other Life Support…” If he or she only wishes life support to be administered at the discretion of the Health Care Provider in charge of his or her care, then the Patient must initial the statement “I Want Life Support…” If the Patient is at the end of his or her life and wants to be allowed to die naturally, then he or she should initial the blank line attached to the words “I Do Not Want Life Support.” 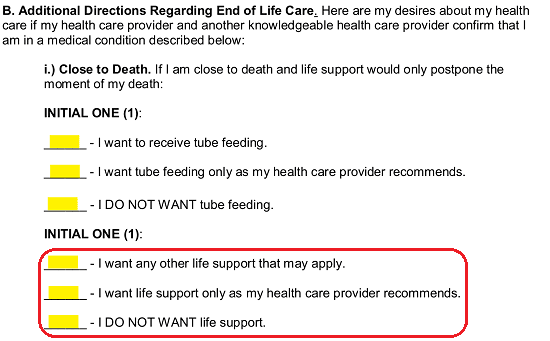 When the Patient is faced with permanent unconsciousness, doctors will seek consultation on his or her feelings regarding living in this condition. In “II.) Permanently Unconscious,” the Patient will be presented with a few statements the first set of three will attempt to define how he or she feels about receiving the nutrients required to live through a tube when permanently unconscious (unable to wake up). The Patient should initial the first statement if he or she wishes to receive nutrients through a tube, initial the second statement if he or she only wishes to receive tube feeding when unconscious as per the recommendations of his or her current health care provider. If the Patient does not wish to prolong his or her life by receiving nutrients artificially (when permanently unconscious) then he or she should in initial the final statement.
When the Patient is faced with permanent unconsciousness, doctors will seek consultation on his or her feelings regarding living in this condition. In “II.) Permanently Unconscious,” the Patient will be presented with a few statements the first set of three will attempt to define how he or she feels about receiving the nutrients required to live through a tube when permanently unconscious (unable to wake up). The Patient should initial the first statement if he or she wishes to receive nutrients through a tube, initial the second statement if he or she only wishes to receive tube feeding when unconscious as per the recommendations of his or her current health care provider. If the Patient does not wish to prolong his or her life by receiving nutrients artificially (when permanently unconscious) then he or she should in initial the final statement. 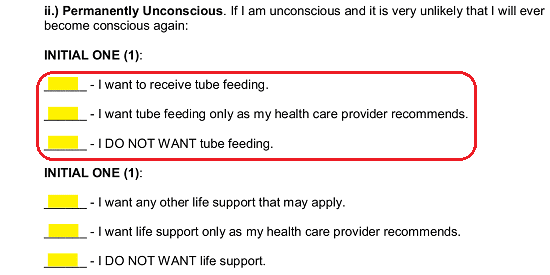 The next area in this section will need the Patient to define his or her feelings regarding life support when he or she is rendered unconscious permanently. Here, the Patient must initial the first statement to allow life support, the second statement to allow the tending physician to make the decision, or the third statement if he or she does not wish to receive life support if diagnosed as permanently unconscious.
The next area in this section will need the Patient to define his or her feelings regarding life support when he or she is rendered unconscious permanently. Here, the Patient must initial the first statement to allow life support, the second statement to allow the tending physician to make the decision, or the third statement if he or she does not wish to receive life support if diagnosed as permanently unconscious. 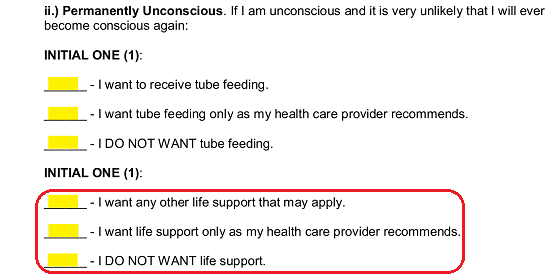
6 – The Patient’s Directives Regarding Advanced Progressive Illness Should Be Included
Next, in “III.) Advanced Progressive Illness,” the Patient should document his or her preferences if he or she is rendered permanently unable to communicate (i.e. unconsciousness, incapacitation) or remain conscious, is at the end of his or her life, and is in the advanced stage of a terminal illness. The first set of statements in this section will aid the Patient in dictating whether or not he or she should receive tube feeding when faced with this scenario. If he or she wishes to be fed nutrients through a tube when necessary, then the Patient should initial the first statement. If the Patient prefers the health care provider to make this decision, then the second statement should be initialed. If, on the other hand, the Patient does not wish to receive any nutrients in an artificial manner (through a tube) then he or she should initial the third statement. 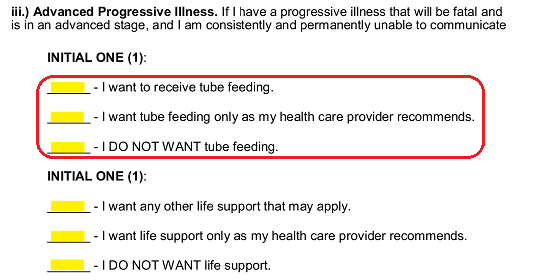 Now, the Patient will need to define his or her feelings in allowing life support to be administered if he or she is in the advanced stages of a fatal disease and is either permanently unconscious or completely unable to communicate. If he or she would like the health care provider to administer life support when necessary so that his or her life may be extended then, the Patient must initial the first statement. The Patient may wish the healthcare provider to make this decision. If so, then the Patient should initial the second statement. If life support should not be administered in such a scenario, then the Patient should initial the “I Do Not Want Life Support” statement.
Now, the Patient will need to define his or her feelings in allowing life support to be administered if he or she is in the advanced stages of a fatal disease and is either permanently unconscious or completely unable to communicate. If he or she would like the health care provider to administer life support when necessary so that his or her life may be extended then, the Patient must initial the first statement. The Patient may wish the healthcare provider to make this decision. If so, then the Patient should initial the second statement. If life support should not be administered in such a scenario, then the Patient should initial the “I Do Not Want Life Support” statement. 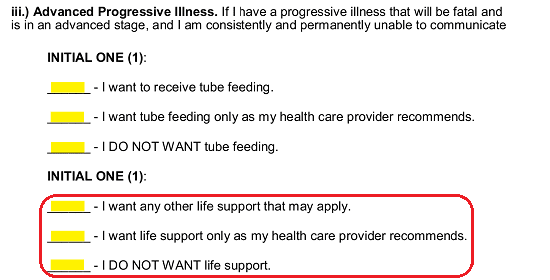 In some cases, the Patient may be suffering a great deal. “IV.) Extraordinary Suffering” will need the Patient’s directives when he or she has suffered a fatal medical event where life support will not benefit his or her medical condition and cause “Permanent And Severe Pain.” If the Patient would wish to receive his or her nutrients through a tube (if required to remain hydrated and well fed) then the Patient should initial the blank line preceding “I Want To Receive Tube Feeding” in this section. If this decision should be left to the Health Care Provider, then the Patient’s initials should be presented on the second blank line. If no tube feeding will be allowed in such a scenario then the Patient should initial the last statement.
In some cases, the Patient may be suffering a great deal. “IV.) Extraordinary Suffering” will need the Patient’s directives when he or she has suffered a fatal medical event where life support will not benefit his or her medical condition and cause “Permanent And Severe Pain.” If the Patient would wish to receive his or her nutrients through a tube (if required to remain hydrated and well fed) then the Patient should initial the blank line preceding “I Want To Receive Tube Feeding” in this section. If this decision should be left to the Health Care Provider, then the Patient’s initials should be presented on the second blank line. If no tube feeding will be allowed in such a scenario then the Patient should initial the last statement. 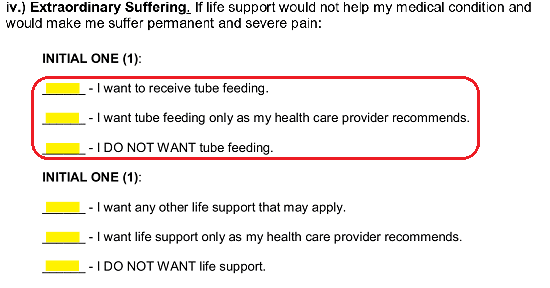 The issue of life support will be a concern when the Patient is faced with “Extraordinary Suffering,” incapacitated, and near the end of his or her life. If the Patient wishes to receive all life support procedures that can be applied in this situation, then he or she should initial the first statement. If the Patient wishes that such a decision be placed in the hands of the health care provider, the second statement will need to be initialed by the Patient. If the Principal does not wish life support to be employed in this scenario, then he or she should initial the third statement.
The issue of life support will be a concern when the Patient is faced with “Extraordinary Suffering,” incapacitated, and near the end of his or her life. If the Patient wishes to receive all life support procedures that can be applied in this situation, then he or she should initial the first statement. If the Patient wishes that such a decision be placed in the hands of the health care provider, the second statement will need to be initialed by the Patient. If the Principal does not wish life support to be employed in this scenario, then he or she should initial the third statement. 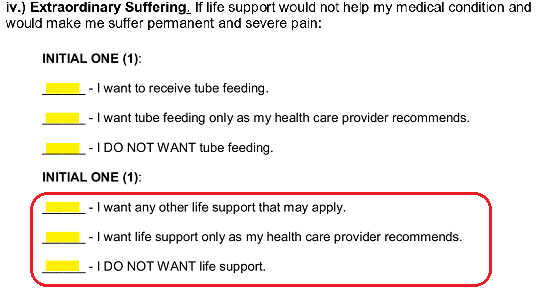
7 – Additional Instructions May Be Attached To This Paperwork
The Patient may have additional restraints, provisions, instructions, preferences, or decisions applied in various scenarios that have not been dealt with above. For instance, he or she may have to observe his or her religion, belief system, or ethical values regarding certain treatments. As per “C.) Additional Instruction” such directives should be included via an attachment. Any such attachment will “…Serve As Guidelines For Health Care Providers…” and can be as specifically worded as the Patient wishes. 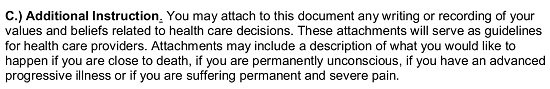
8 – The Patient And Health Care Representative(s) Actions Are Required This Document’s Execution
Only after this form has been completed and any attachments provided should the Principal (or Patient) turn his or her attention to the fifth article “V. My Signature.” Here, the Patient will officially draft the information listed above as his or her wishes. This can only be done when he or she signs the “My Signature” line and provides the signature date on the “Date” line before either a Notary Public or two Witnesses. Once the Patient has signed and dated this paperwork it should be turned over to either the Notary Public or the Witnesses present. 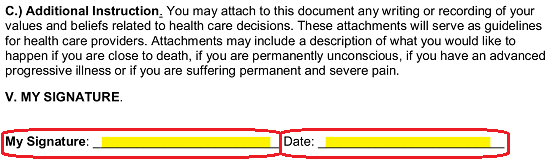 The section labeled “A.) Notary” has been included strictly for the notarization process which only a Notary Public can conduct. He or she will verify several facts (location, date, present parties) and provide his or her credentials (signature, title, commission expiration date, and stamp). If no Notary Public is present, then the two Witnesses will take control of this document.
The section labeled “A.) Notary” has been included strictly for the notarization process which only a Notary Public can conduct. He or she will verify several facts (location, date, present parties) and provide his or her credentials (signature, title, commission expiration date, and stamp). If no Notary Public is present, then the two Witnesses will take control of this document. 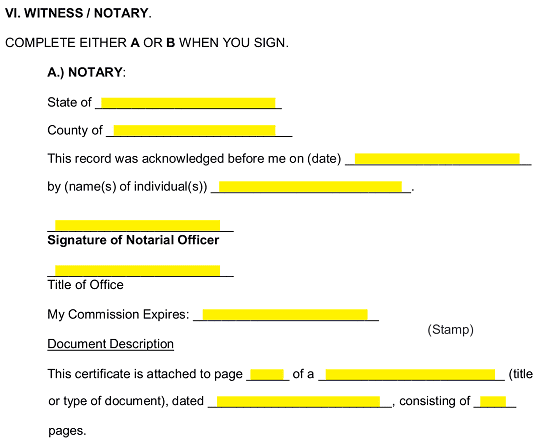 If the Patient’s signature is observed by two Witnesses, then each one must read the statement in the “B.) Witness Declaration” statement. Once done each Witness must print his or her name on either the “Witness Name #1” line or “Witness Name #2” line. Sign his or her name to the appropriate “Signature” line and record the signature date on the line “Date.”
If the Patient’s signature is observed by two Witnesses, then each one must read the statement in the “B.) Witness Declaration” statement. Once done each Witness must print his or her name on either the “Witness Name #1” line or “Witness Name #2” line. Sign his or her name to the appropriate “Signature” line and record the signature date on the line “Date.”
Each Health Care Representative named in this document must show his or her acknowledgment and his or her acceptance of the Health Care Representative role by supplying his or her “Printed Name,” “Signature,” and signature “Date.” in the appropriate areas. The first signature area in “VII. Acceptance By My Health Care Representative” is under the heading “Health Care Representative.”
The next two headings “First (1st) Alternate Health Care Representative” and “Second (2nd) Alternate Health Care Representative are for the back-up agents named in this document. Each one should identify his or her designation then provide the required items (“Printed Name,” “Signature,” and “Date”).